
Are PTSD and Sleep Apnea connected?
Psychogenic non-epileptic attacks (PNEA) are behaviors described as a sudden, violent outburst or a fit of violent action or emotion. These attacks resemble epileptic seizures, but are caused by underlying psychological factors rather than by neurological or biomedical ones.

Sleep apnea and PTSD linked to poor quality of life Study
Een veelvoorkomend symptoom van conversiestoornis is PNEA (Psychogene Niet-Epileptische Aanvallen)* of spanningsaanvallen. Dit betekent dat je aanvallen hebt die erg lijken op epilepsie, maar ze gaan niet samen met epileptiforme activiteit in de hersenen.
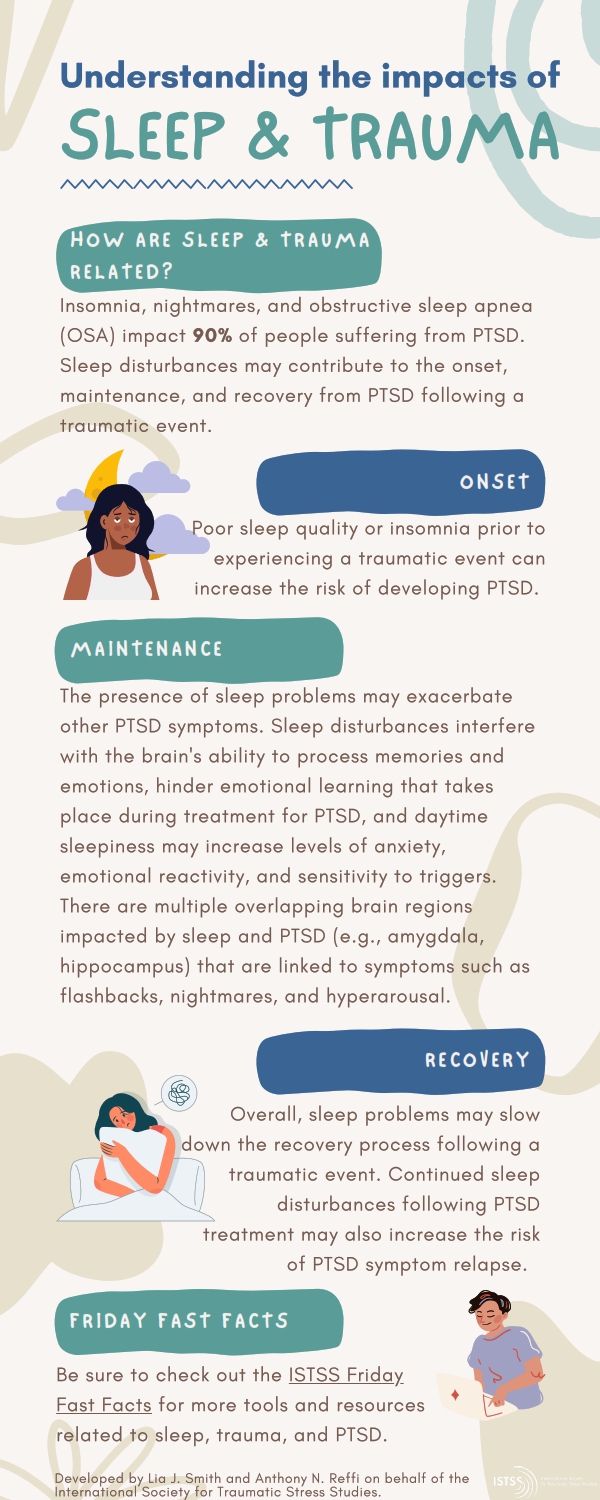
ISTSS Public Resources
Beyond the PTSD criterion symptoms of insomnia and nightmares, 40% to 98% of veterans with PTSD also have a co-occurring sleep disturbance such as obstructive sleep apnea (OSA), periodic leg movement disorder, sleep terrors, or nocturnal anxiety attacks. 4 - 6. OSA is one of the most common sleep disturbances, affecting between 5% and 10% of.

Oorzaken van PTSS en de risicofactoren bondig weergegeven.
Volwassenen met psychogene niet-epileptische aanvallen (PNEA) Patiënten kunnen aanvallen hebben die sterk op epileptische aanvallen lijken, maar dat niet zijn. Zulke aanvallen laten dan geen elektrische ontladingen in de hersenen zien. Ook is er geen sprake van andere storingen in het lichaam, zoals bij flauwvallen of bij hartritmestoornissen.

Understanding PTSD and Sleep Apnea
Conclusions: In the absence of a clear precipitating brain injury, approximately one in six patients intubated for emergent convulsive symptoms had PNEA rather than SE. Although PNEA cannot be diagnosed only by the presence of these risk factors, these simple characteristics could raise clinical suspicion for PNEA in the appropriate setting.
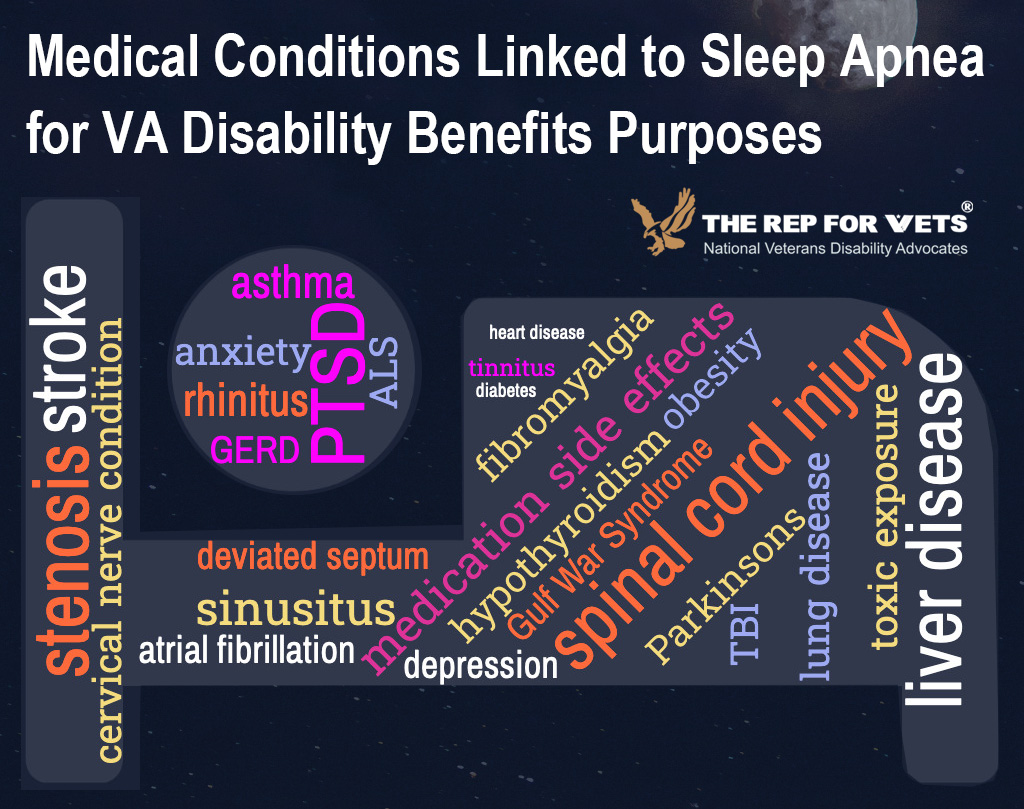
How to Claim Sleep Apnea Secondary to PTSD Rep for Vets
Psychogenic non-epileptic attacks (PNEA) are behaviors described as a sudden, violent outburst or a fit of violent action or emotion. These attacks resemble epileptic seizures, but are caused by underlying psychological factors rather than by neurological or biomedical ones. What makes PNEA different from other non-epileptic conditions, which.

Sleep Apnea Secondary to PTSD? It’s time to start thinking outside the box...
Pseudoseizure is an older term for events that appear to be epileptic seizures but, in fact, do not represent the manifestation of abnormal excessive synchronous cortical activity, which defines epileptic seizures. They are not a variation of epilepsy but are of psychiatric origin. Other terms used in the past include hysterical seizures, psychogenic seizures, and others. The most standard.
Top 3 Tips to Service Connect Sleep Apnea Secondary to PTSD Is There Really a Connection? (The
Wetenschappelijk onderzoek bevestigt dat het onderscheid maken tussen PNEA en epilepsie één van de meest uitdagende opdrachten is voor de hulpverlener (Wood et al., 2004). Er ligt gemiddeld zeven jaar tussen de manifestatie van PNEA-klachten en het stellen van de juiste diagnose door een hulpverlener (Bodde et al., 2009b).

Young Veterans Are Prone to Higher Risk of Sleep Apnea with PTSD
Sleep-disordered breathing can be a sign of untreated OSA, which is associated with worse symptoms of PTSD, as well as an increased risk of heart failure, dementia, and certain cancers. Sleep-disordered breathing is present in 95% of individuals who evacuated a fire, and 91% of victims who experienced consecutive crimes.

Top 3 Tips to Service Connect Sleep Apnea Secondary to PTSD Is There Really a Connection? (The
Readily defined as symptoms consistent with posttraumatic stress disorder (PTSD), but that occur earlier than 30 days after experiencing the traumatic event, posttraumatic stress syndrome (PTSS) is now acknowledged to be a serious health issue. Even so, PTSS often goes unrecognized until an official.

Clinical Importance of Sleep Disturbance as a Treatment Target in PTSD FOCUS
This can be helpful in allowing physicians to definitively identify whether someone has epilepsy or PNEA. Managing Stress . Whether you have PNEA or epilepsy, reducing the stress in your life can be helpful. According to the Epilepsy Foundation, 9 out of 10 people who actively manage their stress believe it has cut their risk of seizures.

Top 3 Tips to Service Connect Sleep Apnea Secondary to PTSD Is There Really a Connection? (The
Background: The empirical literature of network analysis studies of posttraumatic stress symptoms (PTSS) has grown rapidly over the last years.Objective: We aimed to assess the characteristics of these studies, and if possible, the most and least central symptoms and the strongest edges in the networks of PTSS.Method: The present systematic review, conducted in PsycInfo, Medline, and Web of.

sleepapneaandptsd Tabak Law, LLC
Posttraumatic stress disorder (PTSD) is a debilitating anxiety disorder reported in 25% to 30% of individuals experiencing a traumatic event.1Those with this syndrome. present with constellations of symptoms such as intrusive recollection, nightmares, hyperarousal, and disturbed sleep. According to the National Comorbidity Survey, the.

Top 3 Tips to Service Connect Sleep Apnea Secondary to PTSD Is There Really a Connection? (The
Psychogenic nonepileptic attacks (PNEA), also known as psychogenic nonepileptic seizures, dissociative seizures, or pseudoseizures (a term now widely considered pejorative), can be terrifying and frustrating for patients and their families. PNEA are transient episodes of involuntary movements or altered consciousness caused by psychological.

Understanding PTSD and Sleep Apnea
16% of patients intubated for convulsive activity had psychogenic nonepileptic attacks (PNEA). • Six characteristics known on arrival can identify possible PNEA in this setting. • Patients with 5-6 of these risk factors had an 86% chance of having PNEA. • Care should be taken to avoid unnecessary intubation of these at-risk patients.

The Connection Between Sleep Apnea and PTSD Sleep Foundation
Psychogenic nonepileptic seizures (PNES) are nonepileptic events resembling seizures or syncopal attacks. The etiology, epidemiology, clinical features, and diagnosis of PNES are discussed in this review. Management and prognosis are reviewed separately. (See "Psychogenic nonepileptic seizures: Management and prognosis" .)